Will AI replace cancer geneticists?
This essay won a UK Cancer Genetics Group Essay Prize in 2018.
Personalised medicine in clinical practice is today’s reality. In the field of cancer genetics, modern sequencing technologies are used to identify molecular drivers of the disease and to tailor treatment to individuals. Artificial Intelligence (AI), a sophisticated form of data processing that encompasses machine learning, is making its way into this field of medicine in response to the challenge of interpreting complex genomic data. Impressive AI applications across various industries threaten to automate jobs, so should we be raising the white flag on the role of the cancer geneticist?
The rise of Artificial Intelligence in medicine
“There is no precision medicine without AI” - Mesko (2017) [1]
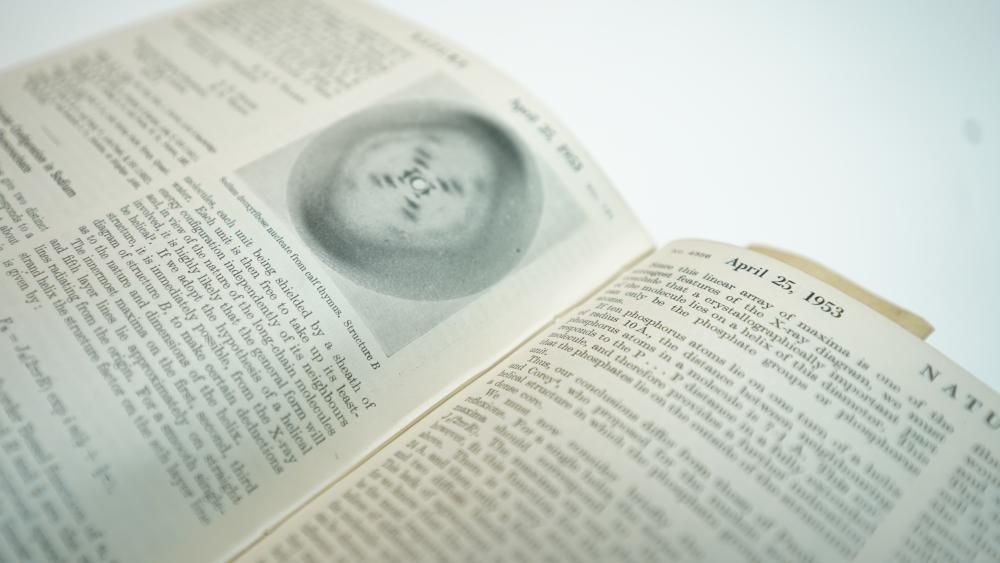
AI algorithms perform tasks that would otherwise require human intelligence [2]. Despite sensationalised headlines, AI is a decades-old field with renewed interest due to developments in computing and data generation. The most referenced branch of AI is Machine Learning (ML), which allows systems to discover patterns in data and make predictions based on this information. Recently a branch of ML inspired by neural networks in the brain, known as deep learning, has facilitated even more accurate outputs by learning from larger datasets.
The amount of data generated by genomics is doubling around every 6 months in tandem with our ability to store, communicate and process information. This relentless progress is driving the need for AI algorithms to transform this data into meaningful insight. Combined with heavy investment in research initiatives, an ageing population and the ethical imperative to invest in healthcare technologies, and cancer is a clear frontrunner for targeted precision medicine. Any number of driver mutations and genomic rearrangements can contribute to the same form of cancer in different individuals. As sequencing tumors with normal DNA has become commonplace for matching patients to treatment, cancer genetics is ever-more reliant on big data and the AI applications used to process it.
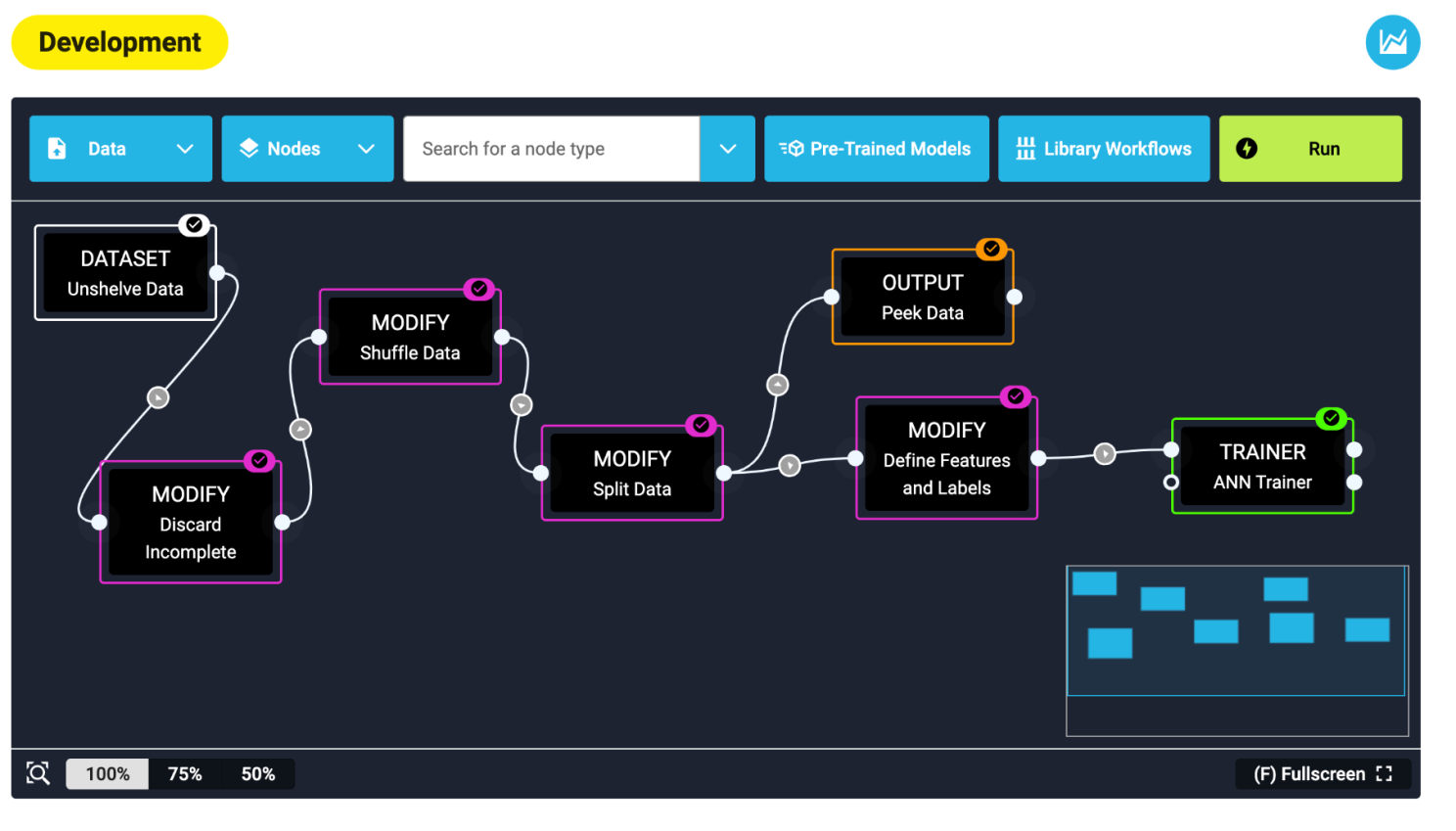
Commercial outfits have recognised the benefit of this and an industry of decision support tools is emerging. Investments from tech powerhouses like Google, Microsoft and IBM are bringing AI research to clinical services. The resources required for analysis typically increase with the amount of genetic data investigated. despite extensive domain expertise, clinicians cannot be expected to account for all the variables in data that indicate the most likely diagnosis or treatment pathway. Research applications have trained AI models to distinguish tissues of origin and tumor types from cancer mutations [6,7] and platforms such as SophiaAI and IBM’s Watson for Genomics platform automate oncology workflows to identify therapeutic options for patients [8,9]. These decision support tools are marketed for their potential to impact genomic medicine using AI, but to determine if this has the potential to supersede clinicians we must first understand the geneticist’s role.
The cancer geneticist under threat?
In 2000, 2011 and 2014, the UK Clinical Genetics Society (CGS) has aimed to define the evolving role of the clinical geneticist [10]. While a number of sub-specialities have emerged over time, the skills relating to patient interaction in this field are essential. Mainstreaming of genomics has increased the demand for talented professionals with the ability to communicate sophisticated analyses to patients and healthcare professionals; enter the 21st century cancer geneticist. Observing the current capacity of AI and concluding that the profession is near extinction makes the assumption that cancer geneticists do no more than work with patient data. They are involved in predictive testing, diagnosis, treatment, case investigation and counselling. They discuss family histories, organise genetic testing, liaise with laboratories to determine results, educate and train colleagues, engage in research, and develop clinical services - This list is by no means comprehensive. While AI may be able to combine data from radiology and pathology in treatment recommendations, regular meetings of oncologists, radiotherapists, surgeons and palliative care clinicians are required to monitor patients and assess treatments over time [11]. In the context of these mandatory multidisciplinary team meetings, clinical geneticists are both informed experts and advocates for patients and their families, communicating to them the complex findings across health domains involved in their care.
Today, the field of Natural Language Processing AI has developed to transcribe speech and respond to queries using chatbots. In oncology research, this technology is being applied to process medical literature [12]. However, it is difficult to imagine a near-future where these tools can empathise with patient concerns while being non-directive in guiding their decision making, as is required of geneticists. Hall (2017) expresses this in a simple aphorism: Clinical geneticists deal with real people [13]. It is unclear that tomorrow’s AI can meet the complexity of counsel clinicians provide. For example, what are the limits of accuracy for a computer aiming to answer a patient’s concerns? Experts answer based on the patient’s emotional state, body language, tone of voice, and personal history. Consultations are influenced by intricate family dynamics, differences in scientific understanding, cultural backgrounds and emotional states, all of which require years of professional practice to address.
AI currently has no bearing on sensitively presenting a cancer diagnosis, or describing a treatment plan in a way that accounts for the patient’s unique situation. The expectation may be that this becomes more plausible if the future brings a switch from narrow to general intelligence. The Turing test defines a machine’s ability to truly replicate human interaction by exhibiting intelligent behaviour indistinguishable from that of a human. Perhaps clinical genetics will be the least of our worries in this event.
Expanding the scope of cancer genetics
Complex molecular data is being generated in cancer research and clinical settings that will require interaction using AI approaches to be translated into clinical insight. Understanding cancer epigenomics, non-coding variation and post-transcriptional measurements are but a few of many hurdles on the road to treatment plans informed by network based statistics. Shrager and Tenenbaum (2014) call this shift ‘Precision oncology 3.0’ [14]. For example as part of the 100,000 Genomes Project, the Genomics England multi-omics project was set up to collect samples for analysis with different omics sets as part of the quantitative methods, ML academic partnerships [15]. Recent studies describe using circulating miRNAs as a class for cancer identification [3], databases combining genetic and clinical data to predict novel cancer drug targets [16] and the identification of metabolites that distinguish individuals with early-stage cancer [17]. AI will likely require cancer geneticists to develop knowledge in novel molecular tests and informatics tools. Cancer geneticists are not detached from accessing this technology and are being enabled to put AI software to practice. For example, OASIS and LinkedOmics [18,19] are web based analysis tools that combine multi omics and clinical phenotype data with statistical associations for clinical prediction. State-of-the-art data mining methods are available to clinicians to visualise and explore omics data. Deep learning algorithms have been shown to diagnose breast cancer metastasis as well as medical professionals, but augmenting algorithmic prediction and clinician input was found to be the most successful [20]. Clearly, AI is has the potential to complement and expand the cancer geneticists role.
Not-so-artificial challenges
Beyond using and interpreting AI-driven applications, clinicians will need a firm grounding in the ethical standards and good practice of working with AI. The ethical and legislative framework for AI in healthcare is in its infancy. AI will not address socioeconomic disparities, or the lack of genomic literacy among patients and care providers. Liability in cases of AI error remains a difficult legislative challenge. Hugh Harvey, a commentator in this space, believes it is unfathomable for owners of AI systems to grant full legal responsibility to machine outputs with patient lives at risk [21]. There is no system with 100% diagnostic accuracy and the consequences of algorithmic error in cancer genetics are a matter of life and death. Even if AI could succeed the clinical geneticist, its application in medicine will be slow, deliberate and highly regulated.
Healthcare systems will need a dramatic overhaul for AI to benefit from the NHS’s comprehensive datasets. Despite a push for digital transformation [22], the health service has not been able to effectively digitise medical records and standardise computer systems. AI will not be the exception to these challenges and building the foundation for a digital health service is a priority. Furthermore, translating these algorithms from research applications to clinical use is non-trivial. Kourou (2015) performed a review of the literature for ML prognosis prediction in cancer and concluded that very few applications truly penetrate clinical practice [3]. Small training sizes, sparse independent validation and dataset quality are existing barriers to implementing AI. Boustros (2018) additionally points out that the seminal paper demonstrating that breast cancer outcomes could be predicted using gene expression was published over a decade ago, and practical uptake has since been limited [23,24]. There are human elements of scientific discovery that AI may never be able to emulate. Many questions critical to advancing cancer genetics have come from experiences with a single infected individual or international collaborations. AI cannot generate hypotheses on its own and patient-led insights do not lend themselves to algorithmic analysis. It is additionally important to note that despite the promise of multi-omics technology, many associations between biomarkers and cancer are only just being understood. Our understanding of ethnic predisposition to genetic variants in cancer is still limited, and there is no precedent for AI models agnostic to the biases in modern clinical databases. Clinical geneticists will be working on these issues for years to come.
Conclusion
AI has the potential to relieve burden of administrative tasks such as ordering tests and compiling notes. Its application in clinical genetics will however be slow and methodical. The scope of clinical genetics expertise will expand and blur the lines between geneticist, radiologist, and informatician. Cancer geneticists will continue to be essential communicators of the complexities of clinical sciences to all stakeholders in healthcare. As ethical guidelines and legal practice on the use of AI become transparent, decision support tools will improve with more sophisticated molecular technologies. With this series of potential events, it holds true that the role of the cancer geneticist will be expanded, not replaced, by AI applications in healthcare.
References
- Mesko B. The role of artificial intelligence in precision medicine. Expert Review of Precision Medicine and Drug Development. Taylor & Francis; 2017;2: 239–241. doi:10.1080/23808993.2017.1380516
- Test van Duin S, Bakshi N. Part 1: Artificial Intelligence Defined - Deloitte - Technology services. In: Deloitte Sweden [Internet]. Mar 2017. Available: https://www2.deloitte.com/se/sv/pages/technology/articles/part1-artificial-intelligence-defined.html
- Kourou K, Exarchos TP, Exarchos KP, Karamouzis MV, Fotiadis DI. Machine learning applications in cancer prognosis and prediction. Comput Struct Biotechnol J. 2015;13: 8–17. doi:10.1016/j.csbj.2014.11.005
- Stephens ZD, Lee SY, Faghri F, Campbell RH, Zhai C, Efron MJ, et al. Big Data: Astronomical or Genomical? PLoS Biol. Public Library of Science; 2015;13: e1002195. doi:10.1371/journal.pbio.1002195
- Hilbert M, López P. The world’s technological capacity to store, communicate, and compute information. Science. 2011;332: 60–65. doi:10.1126/science.1200970
- Marquard AM, Birkbak NJ, Thomas CE, Favero F, Krzystanek M, Lefebvre C, et al. TumorTracer: a method to identify the tissue of origin from the somatic mutations of a tumor specimen. BMC Med Genomics. 2015;8: 58. doi:10.1186/s12920-015-0130-0
- Soh KP, Szczurek E, Sakoparnig T, Beerenwinkel N. Predicting cancer type from tumour DNA signatures. Genome Med. 2017;9: 104. doi:10.1186/s13073-017-0493-2
- Sophia-Genetics. Sophia Genetics - Benefits details. In: Sophia Genetics [Internet]. 2018 [cited 30 Jul 2018]. Available: https://www.sophiagenetics.com/hospitals/benefits/benefits-details.html
- IBM. IBM Watson Health - Oncology and Genomics. In: IBM Watson Health [Internet]. Aug 2018 [cited 2 Aug 2018]. Available: https://www.ibm.com/watson/health/oncology-and-genomics/genomics/
- The Clinical Genetics Society. The Evolving Role of the Clinical Geneticist [Internet]. 2014 Nov. Available: http://www.clingensoc.org/media/954931/theevolvingroleoftheclinicalgeneticist_29.07.15.pdf
- Morement H, Harrison R, Taylor-Robinson SD. The multidisciplinary team meeting in the UK from the patients’ perspective: comments and observations from cholangiocarcinoma patients and their families. Int J Gen Med. 2017;10: 305–310. doi:10.2147/IJGM.S145029
- Yim W-W, Yetisgen M, Harris WP, Kwan SW. Natural Language Processing in Oncology: A Review. JAMA Oncol. 2016;2: 797–804. doi:10.1001/jamaoncol.2016.0213
- Hall JG. The Clinic Is My Laboratory: Life as a Clinical Geneticist. Annu Rev Genomics Hum Genet. Annual Reviews; 2017;18: 1–29. doi:10.1146/annurev-genom-091416-035213
- Shrager J, Tenenbaum JM. Rapid learning for precision oncology. Nat Rev Clin Oncol. 2014;11: 109–118. doi:10.1038/nrclinonc.2013.244
- Genomics-England. Multi-Omics samples. In: Genomics England [Internet]. 2018 [cited 30 Jul 2018]. Available: https://www.genomicsengland.co.uk/about-gecip/for-gecip-members/multi-omic-samples/
- Bulusu KC, Tym JE, Coker EA, Schierz AC, Al-Lazikani B. canSAR: updated cancer research and drug discovery knowledgebase. Nucleic Acids Res. 2014;42: D1040–7. doi:10.1093/nar/gkt1182
- Gaul DA, Mezencev R, Long TQ, Jones CM, Benigno BB, Gray A, et al. Highly-accurate metabolomic detection of early-stage ovarian cancer. Sci Rep. 2015;5: 16351. doi:10.1038/srep16351
- Fernandez-Banet J, Esposito A, Coffin S, Horvath IB, Estrella H, Schefzick S, et al. OASIS: web-based platform for exploring cancer multi-omics data. Nat Methods. 2016;13: 9–10. doi:10.1038/nmeth.3692
- Vasaikar SV, Straub P, Wang J, Zhang B. LinkedOmics: analyzing multi-omics data within and across 32 cancer types. Nucleic Acids Res. 2018;46: D956–D963. doi:10.1093/nar/gkx1090
- Wang D, Khosla A, Gargeya R, Irshad H, Beck AH. Deep Learning for Identifying Metastatic Breast Cancer [Internet]. arXiv [q-bio.QM]. 2016. Available: http://arxiv.org/abs/1606.05718
- Harvey H. Why AI will not replace radiologists. In: Medium [Internet]. 24 Jan 2018. Available: https://towardsdatascience.com/why-ai-will-not-replace-radiologists-c7736f2c7d80
- Matthew Honeyman Phoebe Dunn. A digital NHS: An introduction to the Digital agenda and plans for implementation [Internet]. 2016. Available: https://www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/A_digital_NHS_Kings_Fund_Sep_2016.pdf
- Boutros PC. The path to routine use of genomic biomarkers in the cancer clinic. Genome Res. 2015;25: 1508–1513. doi:10.1101/gr.191114.115
- van ’t Veer LJ, Dai H, van de Vijver MJ, He YD, Hart AAM, Mao M, et al. Gene expression profiling predicts clinical outcome of breast cancer. Nature. 2002;415: 530–536. doi:10.1038/415530a